Author Bio: Since 1981, Andrew Karam, PhD, CHP has worked primarily in areas related to radiation safety as a radiation safety professional, a scientist and professor, a consultant, or an instructor. He is currently a Fellow of the Health Physics Society and a Homeland Security Scientific Advisor for Mirion Technologies. He is also a writer, with over 200 encyclopedia articles, a variety of scientific and technical articles, several books in print, and an 8-book series (Controversies in Science, Facts on File) in the works. Learn more at www.andrewkaram.com.
After Fukushima: Training Medical Responders to Care for Contaminated Patients
In early April 2011 I got a phone call from a non-governmental organization (NGO) called NYC Medics – they were wondering if I was willing to travel to Japan to help provide training for medical and emergency responders who were working in and caring for patients coming from areas contaminated by radioactive fallout from the reactor meltdowns. It took me about two seconds to agree – a week or so later I was on an ANA flight to Tokyo, to meet up with the other two members of our group. I brought with me some of my radiation detectors and a dosimeter for each person in our group – I assumed the informal role of Radiation Safety Officer for our group while we were in the Fukushima area.
In a few phone calls (in those pre-Zoom days) with our Japanese hosts and NYC Medics we settled on a course of action when we arrived. Our mission was to provide training, but we agreed that we wanted to work from the standpoint of personal knowledge of conditions in the affected areas as opposed to simply telling attendees “This is what the International Atomic Energy Agency says” or “This is what the Japanese government says.” So we agreed to start our trip with three days in the areas that were slammed with the tsunami and subject to fallout from the reactor meltdowns. (I was hoping to visit the nuclear power station, but I suspect my colleagues (a physician and an expert in the psychosocial impacts of WMD and similar disasters) were somewhat relieved.) After returning to Tokyo, our plan was to spend a day developing our training and the last week or so of our time in Japan would be spent presenting it to a variety of audiences throughout northern Japan – as far south as Kamakura and as far north as Sapporo on the island of Hokkaido.
The time we spent in the areas affected by the tsunami and radioactive fallout was heartbreaking. Areas that had been inundated by the tsunami were devastated – acres of mud littered with debris, reefs of battered cars, and the occasional shell of a building left standing. It was sobering to realize that each car represented one or more people trying to flee the tsunami who had failed; even more sobering was the field we passed that had a line of men, each holding a bamboo pole, probing the mud for bodies. We spent three days in this area, visiting shelters, meeting with mayors, talking with physicians, and trying to wrap our minds around what had happened.
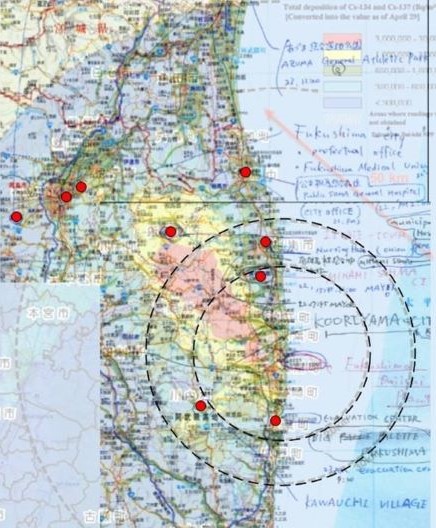
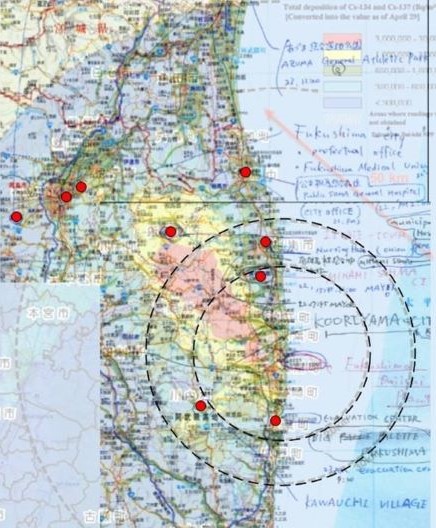
One of my objectives was to make what radiation measurements I could, and it was clear that we spent much of our time in areas where the fallout plume had settled to the ground. Not only were radiation dose rates close to 100 times higher than what’s normal in most of Japan (as high as about 0.5 mR/hr), but I was also able to identify I-131 and I-133, both with half-lives far too short to occur naturally and both produced in copious quantities by nuclear fission. I also identified Cs-137 and Cs-134, two other fission products, and a later analysis of the spectra I collected revealed a few more nuclides as well.
We returned to Tokyo on one of the first shinkansen (bullet trains) to leave Sendai after the earthquake and spent the next day figuring out what we wanted to say and how we wanted to say it. As the group’s health physicist I spoke about how to safely treat contaminated patients, our physician talked about the medical effects of radiation and contamination exposure, and our psycho-social researcher talked about those aspects of major radiological events. And, since we had some lectures that were to be one hour and some that were slated for two, we also discussed whether or not to have two separate sets of slides (we finally decided to go with a single set, just to include more details for the longer lectures). Finally, we also decided to avoid lecturing our audience but, rather, to treat our sessions more as a sort of refresher training.
For my part of the training, I focused on good radiological work practices when working with contaminated patients. Contamination control, for example – I discussed the fact that Alexander Litvenenko was shedding Po-210 with every hair shed from his head and his body, unbeknownst to any of those caring for him. In spite of that, none of the hospital staff had a significant intake of polonium because they were simply taking the normal precautions that they took with any patients suffering from an unknown ailment; that the standard precautions they already knew how to take were perfectly capable of protecting them from radioactive contamination as well as from the more common microbes. Then I’d ask them if they ever cared for nuclear medicine patients – in every group there were several – and I’d mention that the lowest diagnostic radiopharmaceutical dose carried more radioactivity than even most heavily contaminated patients. The message was that we weren’t trying to teach them anything new – just to remind them that they already knew what to do, they just might not realize it.

I went through the standard time-distance-shielding explanations as well as other basics (types of radiation, health effects, natural radiation, and so forth) as well as a quick discussion of the radiological conditions we’d seen in the Fukushima area. But the main focus of my part of the lecture was a review of good radiation safety work practices that was aimed at helping them to feel comfortable caring for their patients. In large part, this was because of surveys conducted shortly after the September 11 attacks, showing that up to 30% of medical responders might decide not to go to work in the event of a radiological attack, citing fears of the health effects on them and their families – we felt it important to try to assuage any such concerns among those in our audience.
The medical discussion came next, beginning with a brief discussion of the manner in which radiation affects the body and the amount of exposure required to cause problems; our physician also reviewed the nuclides we had identified during our time in the plume area and how those affected the body. She also spent some time talking about recognizing radiation injury, the symptoms of Acute Radiation Syndrome, and a bit about radiation’s role in inducing cancers, as well as the normal latency period for such cancers. And then she closed this part with a brief discussion of the effects of radiation on pregnancy; there are estimates that, in the aftermath of Chernobyl, European women had over 100,000 unnecessary therapeutic abortions, primarily because their physicians didn’t have a good understanding of the reproductive effects of radiation exposure – given our audience, we wanted to make sure they all had a good understanding of the topic.
Finally, we closed with a discussion of the psychological effects noted in earlier radiological and nuclear accidents, helping the audience to understand what to look for in their patients as well as among their patients’ families. Here, too, we could draw on what we had seen earlier during our visits to the towns, shelters, and hospitals, as well as how people often reacted to being screened, being ordered to evacuate, and so forth. This part closed with a discussion of healthcare professionals and how they often reacted to working with patients whom they feared might pose a risk to them. After we were done, we opened the floor for any questions.
Over the course of about a week we gave 7 presentations in five different cities to groups as small as 50 and as large as 250 people – we figured we reached over 1000 people in these talks. One concrete outcome was that the organization that sponsored our time in Japan (and the one that had asked NYC Medics for our help) told us that they had authorized admitting up to 5000 patients from contaminated areas to their hospitals – this freed up needed beds closer to the accident site and elsewhere in Japan.

One of the biggest adjustments for all of us was working with translators – we never did decide if it was easier to work with simultaneous or sequential translation. Early on we realized that it was important to sit down with our translators before each lecture (we had different sets for each venue) to make sure they understood the scientific terminology as well as finding out their preferences and how we could make their job easier. It was an interesting experience for all of us!
When all was said and done, we’d spent 12 days in Japan, most of which we were busy for 12-16 hours. We logged over 50 aftershocks stronger than magnitude 5, with the strongest being a 6.0 our first night there (I slept through it), and we each picked up more radiation dose on the flights over and back than during our time on the ground. I’m not sure about my colleagues – I was so tired that I slept through virtually the entire flight back from Tokyo to New York. All in all it was exhausting – but we all agreed it was also one of the high points of our careers. One that we hope to never repeat.
The views, thoughts, and opinions expressed in the text belong solely to the author, and do not necessarily reflect the views and opinions of Versant Physics.