We are often asked questions about applying for or changing licenses to possess and use radioactive materials. There are many different types of licenses; choosing amongst them can be confusing. In this post, we will discuss four common types.

With some exceptions, approval by a regulatory agency (U.S. Nuclear Regulatory Commission or equivalent state agency), in the form of a license, is required to use and/or dispose of radioactive materials.
The type of license authorizing the purchase, possession, use, and disposal of radioactive materials is based on several factors:
- Type, form and quantity of radioactive materials requested
- Proposed use(s)
- Experience of the proposed licensee with managing the use of radioactive materials
Types of licenses include, but are not limited to:
- Limited scope specific academic and research and development
- Limited scope specific medical use
- Broad scope specific
- Broad scope specific medical use
In this post, we will discuss the regulations under which the U.S. Nuclear Regulatory Commission (NRC) issues two common types of licenses: (i) limited scope specific and (ii) broad scope specific. Some states, called Agreement States, have the authority under NRC regulations to issue licenses. Their regulations are equivalent to NRC regulations.
1. Limited Scope Licenses
These licenses are issued to applicants subject the following limitations:
- Radionuclides
- Specified chemical and physical form(s)
- Possession limits
- Proposed use(s)
- Radiation Safety Officer (RSO)
- Authorized User(s)
- Location(s) of use
The RSO’s training and experience should be applicable to and generally consistent with the types and quantities of licensed materials listed on the license. Authorized users (AUs) must have adequate training and experience with the types and quantities they intend to use (NUREG 1556, Vol. 7, Rev. 1). The applicant must submit to the regulatory agency for review and approval the specific training and experience of each proposed user and the facilities and equipment available to support each proposed use.
If the licensee wishes to change any of these limitations or add or remove an Authorized User (AU), permission must be sought from the issuing regulatory agency to amend the license.
Medical Licenses – general comments
Licensing for the use of radioactive materials to diagnose and treat human disease is subject to more complex regulations than the academic and research and development licenses described above. A wide variety of radionuclides and physical and chemical forms are used for a multitude of purposes in human medicine. Consequently, AUs and the RSO must meet specific and extensive training and experience criteria focusing on the type, form, and quantity to be used as well as the intent of the use (diagnosis vs. treatment).
An AU is charged with the responsibility for (NUREG 1556 Vol. 9, Rev. 3)
- radiation safety commensurate with use of radioactive materials;
- administration of a radiation dose or dosage and how it is prescribed;
- direction of individuals under the AU’s supervision in the preparation of radioactive materials for medical use and in the medical use of radioactive materials; and
- preparation of a written directive, if required.
To be named as an AU on a medical license, the individual must satisfy one or more of the requirements outlined in Subparts D, E, F, G or H of 10 CFR 35. In general, this requirement can be met by:
- being board certified in a specialty medical discipline appropriate to the intended use that is recognized by the Commission or Agreement State; or
- being named as an AU on another license issued by the Commission or Agreement State for the same or similar type, form, and quantity of radioactive materials in question; or
- having completed training and experience as specified in the regulations.
The RSO on a medical license must satisfy the training and experience requirements outlined in 10 CFR 35.50:
- be certified by a specialty board whose certification process has been recognized by the Commission or an Agreement State; or
- have completed a structured educational program as outline in 10 CFR 35.50(b); or
- be a medical physicist who is certified by a specialty board recognized by the Commission or an Agreement State, has experience with the radiation safety aspects of similar types of radioactive materials for which the licensee seeks approval and has training in the radiation safety, regulatory issues, and emergency procedures for the types of use for which a licensee seeks approval; or
- be a medical AU, authorized medical physicist, or authorized nuclear pharmacist identified on a Commission or an Agreement State license, a permit issued by a Commission master material licensee, a permit issued by a Commission or an Agreement State licensee of broad scope, or a permit issued by a Commission master material license broad scope permittee, has experience with the radiation safety aspects of similar types of use of byproduct material for which the licensee seeks the approval and Is an authorized user, authorized medical physicist, or authorized nuclear pharmacist identified on a Commission or an Agreement State license, a permit issued by a Commission master material licensee, a permit issued by a Commission or an Agreement State licensee of broad scope, or a permit issued by a Commission master material license broad scope permittee, has experience with the radiation safety aspects of similar types of use of byproduct material for which the licensee seeks the approval.
2. Limited Scope Specific Medical Licenses
A specific license of limited scope may be issued to private or group medical practices and to medical institutions. Each type, form, quantity and use and condition of use of radioactive materials as well as the RSO and AU(s) are named on the license (NUREG 1556 Vol. 9, Rev. 3). These licenses may also be issued to an entity requesting authorization to perform mobile medical services and certain non-medical activities such as self-shielded blood irradiators. Changes to any of these specifications or conditions must be requested and approved by amendment.
Research Involving Human Subjects
“Medical use” of radioactive materials includes administration to human research subjects. A license condition authorizing such research is not required if the research is conducted, funded, supported or regulated by a Federal Agency that has implemented the Federal Policy for the Protection of Human Subjects. Otherwise, the licensee must apply for and receive an amendment before conducting such research. In all cases, licensees must obtain informed consent from the human subjects and prior review and approval by an Institutional Review Board. All research involving human subjects must be conducted only with the radioactive materials listed in the license and for the uses authorized in the license (NUREG 1556, Vol. 9, Rev. 3).
Research involving human subjects may be conducted under either limited scope or broad scope specific licenses.
3. Broad Scope Specific Licenses
Broad scope specific licenses generally authorize possession and use of a wide range of radioactive materials. Because regulatory agencies grant significant decision-making authority to broad scope licensees through the license, a broad scope license is not normally issued to a new licensee. An applicant for a broad scope license typically has several years of experience operating under a limited scope license and a good regulatory performance history (NUREG 1556 Vol. 11, Rev. 1). Changes to the radiation safety program approved via in-house review and approval by the RSO and/or RSC (see below) do not appear on the license but are subject to review by regulatory agencies during routine inspections.
Title 10 of the Code of Federal Regulations (10 CFR) Part 33, “Specific Domestic Licenses of Broad Scope for Byproduct Material,” provides for three distinct categories of broad scope licenses (i.e., Type A, Type B, and Type C), which are defined in 10 CFR 33.11, “Types of Specific Licenses of Broad Scope.”
Type A
Type A licenses of broad scope are typically the largest licensed programs and encompass a broad range of uses. Licensees use a Radiation Safety Committee (RSC), radiation safety officer (RSO), and criteria developed and submitted by the licensee and approved by the NRC during the licensing process to review and approve all uses and users under the license.
An applicant for a Type A broad scope license must establish administrative controls and provisions related to organization and management, procedures, record keeping, material control, and accounting and management review necessary to ensure safe operations, including:
- establishment of an RSC
- appointment of a qualified RSO
- establishment of appropriate administrative procedures to ensure the following:
— control of procurement and use of byproduct material
— completion of safety evaluations of proposed uses that take into consideration adequacy of facilities and equipment, training and experience of the user, and operating and handling procedures
— review, approval, and recording by the RSC of safety evaluations of proposed uses
- use of byproduct material only by, or under the direct supervision of, individuals approved by the licensee’s RSC
Because these controls and provisions have been established, the applicant may approve in-house, without requesting amendment:
- Authorized Users
- location of use within the confines of the physical location(s) listed on the license
- changes in use of radioactive materials so long as the use is consistent with the license conditions and appropriate safety evaluations have been performed, documented, and approved by the RSC
The requirements for issuance of a Type A broad scope license are described in 10 CFR 33.13, “Requirements for the Issuance of a Type A Specific License of Broad Scope.”
Type B
Type B broad scope licensed programs are normally smaller and less diverse than Type A broad scope programs. Type B broad scope licensees use an RSO and criteria developed and submitted by the licensee and approved by the NRC during the licensing process to review and approve all uses and users under the license. Because the RSO reviews and approves all uses and users under the license, rather than a full RSC, as established for Type A broad scope programs, the types and quantities of byproduct material authorized by the Type B broad scope license are limited to those described in 10 CFR 33.11(b) and 10 CFR 33.100, “Schedule A,” Column I. Generally, the scope of authorization for Type B licenses is limited to the experience and knowledge of the RSO.
Changes to the type, form and quantity of radioactive materials may have to be approved by the regulatory agency by amendment, depending on the specific provisions of the license.
The requirements for issuance of a Type B broad scope license are described in 10 CFR 33.14, “Requirements for the Issuance of a Type B Specific License of Broad Scope.”
Type C
Type C broad scope licensed programs typically are issued to institutions that do not require significant quantities of radioactive material but need the flexibility to possess a variety of different radioactive materials. Users of licensed material under these programs are approved by the licensee based on training and experience criteria described in 10 CFR 33.15(b). The types and quantities of byproduct material authorized by the Type C broad scope license are limited to those described in 10 CFR 33.11(c) and 10 CFR 33.100, Schedule A, Column II, again, considering the unity rule.
While 10 CFR 33.15 does not require Type C broad scope licensees to appoint an RSO, the licensee must establish administrative controls and provisions related to procurement of byproduct material, procedures, record keeping, material control and accounting, and management review to ensure safe operations. This should include the appointment of someone responsible for the day-to-day operation of the radiation safety program, such as an RSO.
Changes to the type, form and quantity of radioactive materials may have to be approved by the regulatory agency by amendment, depending on the specific provisions of the license.
The requirements for issuance of a Type C broad scope license are described in 10 CFR 33.15, “Requirements for the Issuance of a Type C Specific License of Broad Scope.”
4. Broad Scope Medical Licenses
The NRC issues specific licenses of broad scope for medical use (i.e., licenses authorizing multiple quantities and types of byproduct material for medical use under 10 CFR Part 35, as well as other uses) to institutions that (i) have experience successfully operating under a specific license of limited scope and (ii) are engaged in medical research and routine diagnostic and therapeutic uses of byproduct material (NUREG 1556, Vol. 9, Rev. 3). Typically, these are large medical centers/teaching hospitals that have a need to administer or use a wide variety of radionuclides and/or radiopharmaceuticals for diagnosis and therapy. Because these institutions have complex programs, the authority to approve changes in-house makes the program flexible and nimble.
AUs and the RSO on a broad scope medical license must meet the same criteria for training and experience as for a limited scope medical license discussed above.
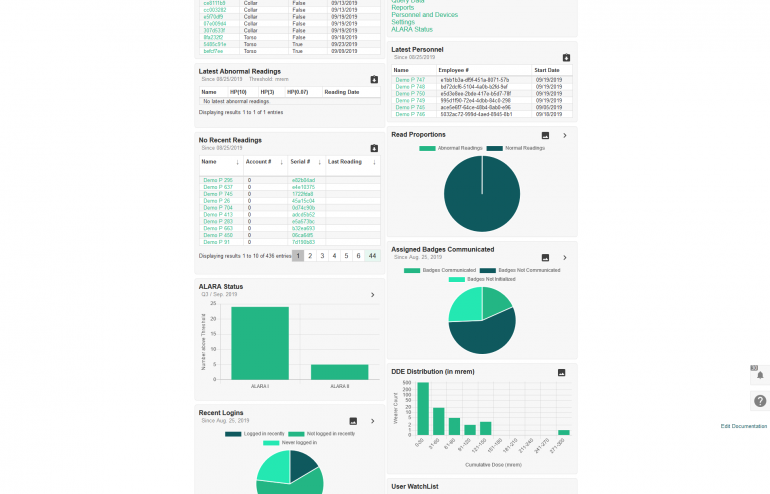
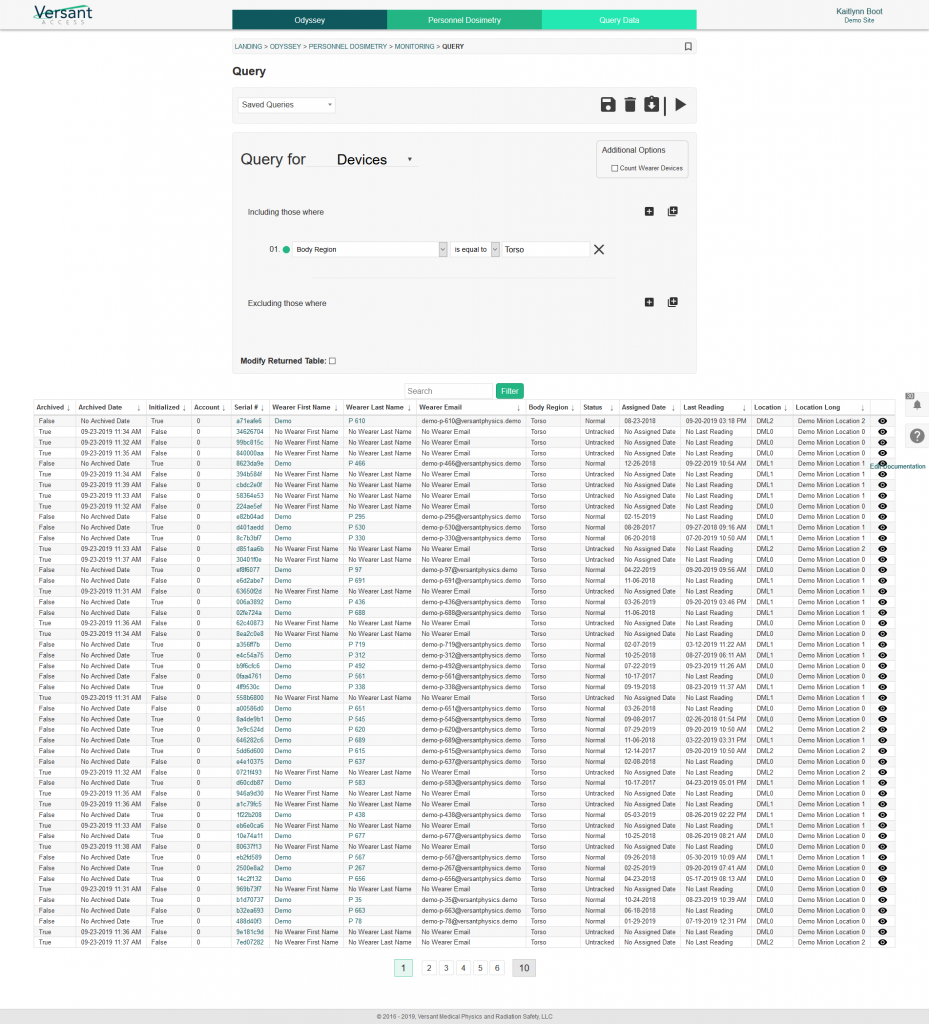
Regulatory Services by Versant Physics
Our team of experienced Radiation Safety Officers can help you navigate the NRC regulations and determine which license type is appropriate for your facility. Contact sales@versantphysics.com to speak to a team member or learn more about our Regulatory services.