Patient safety is a major focus of radiation treatments and diagnostic imaging procedures. However, radiation workers in the healthcare field are also at risk for exposure to unsafe amounts of radiation—primarily scatter radiation—due to the nature of their work.
Protecting healthcare workers from scatter radiation is an important part of a successful radiation safety program. In today’s blog post, we discuss what scatter radiation is, effects on the human body, and four ways to help limit occupational exposures.
What is scatter radiation?
During typical diagnostic imaging procedures such as fluoroscopy, CT, or mammography exams, healthcare workers are exposed to scatter radiation.

Scatter radiation is a type of secondary radiation.1 It occurs when the primary beam from a source such as a CT Scanner, X-Ray, or Fluoroscopy unit interacts with matter. For scatter radiation, the “matter” that X-ray beams are most often interacting with is the patient in a procedure. As the primary beam intercepts the patient’s body tissues, some X-rays will bounce off those atoms to create secondary, specifically scatter, radiation.
Scatter radiation can be moderated through some machine positioning, like the C-Arm. The primary beam for a C-Arm is sent up through the table into a patient before being read by the other side of the machine. In this case, the back scattered radiation produced by the entrance beam below the table is mostly towards the floor and lower extremities of the radiation worker. Scatter coming out of the exit radiation from the patient is also present but reduced in intensity as compared with the entrance scatter below the table. Not all units are designed in this manner, however, and these scattered rays will be present in the imaging room until the diagnostic x-ray machine is turned off.2
What are the effects of scatter radiation on the human body?
Professionals performing diagnostic imaging procedures, such as radiologic technologists, are those most susceptible to scatter radiation emanating from a patient. Scatter radiation does not have as much energy as a primary X-ray beam does but over time it still can cause harm without technologists taking appropriate protective measures. This is a real risk for radiation workers, as they are potentially exposed to scatter radiation multiple times a day while running patients through their diagnostic imaging.
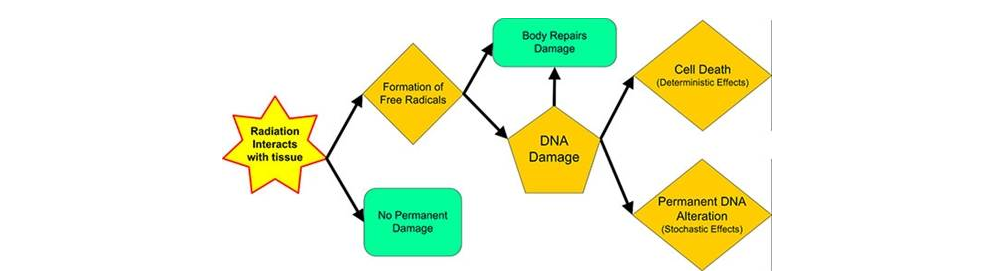
Without appropriate protection, radiation workers will begin to experience adverse health effects from prolonged scatter radiation exposure. This is because radiation has the potential to damage living tissue and organs.3 Severity of damage scope is dependent upon several factors:
- the manner and length of time exposed
- characteristics of the exposed person
- the type of radiation
- any involved radioactive isotopes
- the sensitivity of affected tissue and/or organs
Since scatter radiation exposure is at lower energy and accumulated over longer periods of time (because technologists are performing X-ray procedures as a daily task), the risks of adverse effects are not as severe. However, radiation workers face an increased risk of cancer over a lifetime if protection is not made a priority in the workplace.4
Protection from your occupational exposure
Radiation worker protection should take as much priority as patient protection when it comes to radiation exposure. The ALARA principle is the standard for keeping radiation exposure “As Low As Reasonably Achievable”. As such, following these practices would be our top recommendation for limiting occupational exposure, with a couple additions. Here are the four ways to be best protected from scatter radiation:
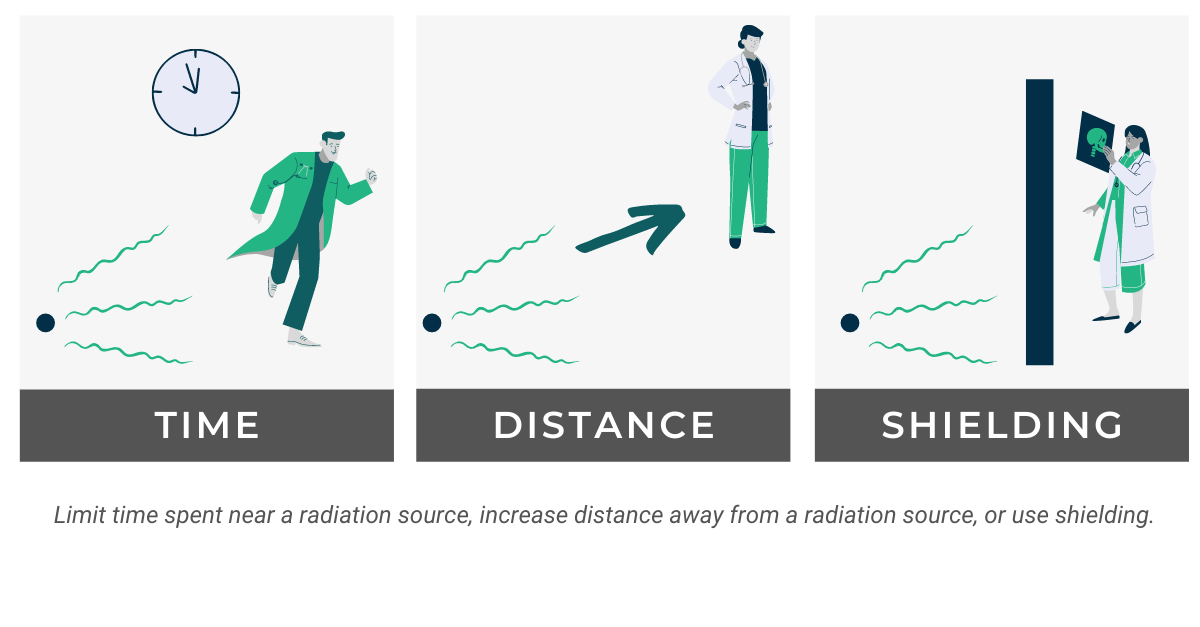
Time
Limit the time that you spend near a radiation source while working. The more time that you are exposed to scatter radiation increases the possibility for a higher overall dose. If you must work near a source of radiation, work as quickly as possible and then leave the area to avoid spending more time around the source than necessary.
Distance
The second ALARA principle, distance, encourages distancing yourself from radiation sources. Radiation exposure decreases with distance, following an inverse square law for a point source. Doubling your distance will cause dose rate to go down by a factor of four. A “general rule of thumb” you can calculate is that any scatter radiation one meter from the side of the patient will be 0.1% of the primary x-ray beam intensity.5 This is helpful to keep in mind when considering how much distance you’re able to maintain during patient treatments.
Shielding

Shielding is the well-known practice of placing a barrier between you and a radiation source for minimizing exposure. The material for these barriers normally depends on radiation source type. For any radiation, though, the shielding should be something that absorbs radiation such as lead, concrete, or water. The practice of shielding can also include personal protective equipment (PPE) directly worn by individuals, such as thyroid shields, radiation protection glasses, and lead vests. For scatter radiation, a combination of moveable shields either suspended from the ceiling or on rollers in addition to fixed table shields are ideal.6 In general, shields are placed close to the source as that allows for a greater solid angle to be covered.
Dosimetry Program
As medicine and medical technology advances, the use of radiation has become more ubiquitous; there is now a greater risk of ionizing radiation exposure for occupational workers. The need for effective radiation monitoring has become more crucial to account for these modern practices.
Radiation dosimeters worn on the body are able to provide a record of absorbed dose from ionizing radiation. Although the measurement of exposure so obtained is not direct protection, being able to track your absorbed dose is essential to the practice of radiation safety. Through regular dose readings, you can know if you’ve reached or are close to reaching the annual NRC occupational dose limits. In the long run, this is a great method for protection against scatter radiation; should you exceed dose limit, you can adjust your work for the rest of the year to avoid further exposure. Thanks to dosimetry programs, radiation workers can stay informed and avoid potential risks better than ever.
The Take-Away
Scatter radiation, even if not as potent as a primary radiation dose, can still have adverse effects over time. To avoid potential increases to your risk of cancer down the road, it’s essential to maintain protective habits when performing diagnostic imaging procedures. Following the ALARA principles and remembering the long-term value of a dosimetry program can keep exposure to scatter radiation and its negative health effects to a minimum.
Versant Physics’ dosimetry management services are available to help your company take that step further in scatter radiation protection. Learn more about our knowledgeable support team and the Instadose family of dosimeters today. For more information regarding shielding, scatter radiation, and applicable policies for a medical radiation safety officer, try our online MRSO or Medical X-Ray courses.
References
- What is primary radiation and secondary radiation? Reimagining Education. Published August 26, 2022. Accessed February 20, 2023. https://reimaginingeducation.org/what-is-primary-radiation-and-secondary-radiation/
- Lambert K. hps.org. Health Physics Society. Accessed February 20, 2023. https://hps.org/publicinformation/ate/q11396.html
- Radiation and health. Who.int. Accessed February 20, 2023. https://www.who.int/news-room/questions-and-answers/item/radiation-and-health
- Morgan WF, Sowa MB. Non-targeted effects induced by ionizing radiation: mechanisms and potential impact on radiation induced health effects. Cancer Lett. 2015;356(1):17-21. doi:10.1016/j.canlet.2013.09.009
- Lovins K. hps.org. Health Physics Society. Accessed February 20, 2023. https://hps.org/publicinformation/ate/q11780.html
- Klein LW. Proper Shielding Technique in Protecting Against Scatter Radiation. Vascular Disease Management. Published June 2021. Accessed February 20, 2023. https://www.hmpgloballearningnetwork.com/site/vdm/commentary/proper-shielding-technique-protecting-against-scatter-radiation