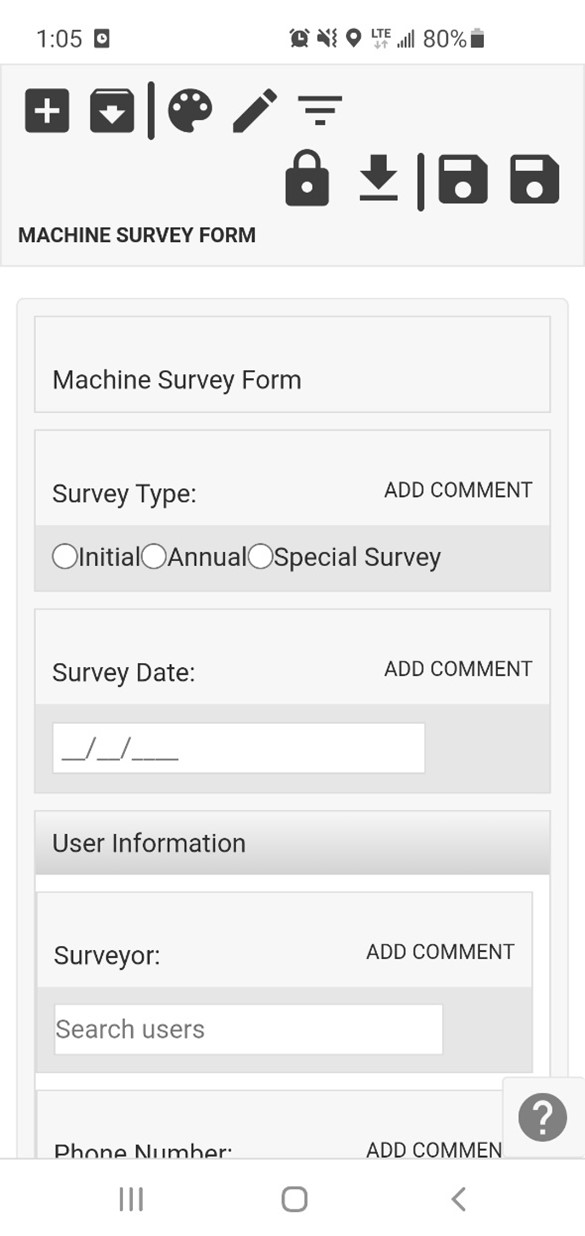
Join us for an interview with our Odyssey Implementation Analyst Katelyn Waters, where we discuss how to carry out certain functions of the Personnel Dosimetry module and answer some of your frequently asked questions.
Odyssey is a radiation safety software suite designed to help RSOs, EHS managers, and Radiation Safety Specialists manage affordable and efficient programs.
KB 00:10: Welcome to Part 1 of our Odyssey how-to series, where we highlight some frequently asked questions about the cloud-based radiation safety software suite and its application in real-world radiation safety programs. Over the next 12 weeks, we’ll be addressing each of Odyssey’s modules, and breaking them down to give a better idea of how they work. My name is KB, and today I’m joined by Odyssey Implementation Analyst Katelyn Waters to discuss the Personnel Dosimetry Module. Thanks for joining me, Katelyn!
Katelyn 00:37: Thanks KB, I’m happy to be here and hopefully we can help answer some of the frequently asked questions that we get for the Personnel Dosimetry module in Odyssey.
KB 00:46: So, the personnel dosimetry module is a key feature of the Odyssey platform. It features customizable widgets and reporting tools that help RSOs and EHS professionals managing a badge program do so in a very efficient way. But how exactly is dosimetry data made available in the module?
Katelyn 01:05: That’s an excellent question, and one of the first that we get whenever we are doing different demonstrations of the software. So, personnel dosimetry does support data from any vendor, but it is primarily designed for Mirion and Landauer. So what it actually does is the software uses a login to either AMP for Mirion or MyLDR for Landauer to view and import that dosimetry information into your account. And so this import happens automatically, we set it up to be daily for Mirion and monthly for Landauer, and so everything’s going to be automatically pulled into the software for you.
KB 01:43: If I have multiple dosimetry accounts can I use this module to manage them?
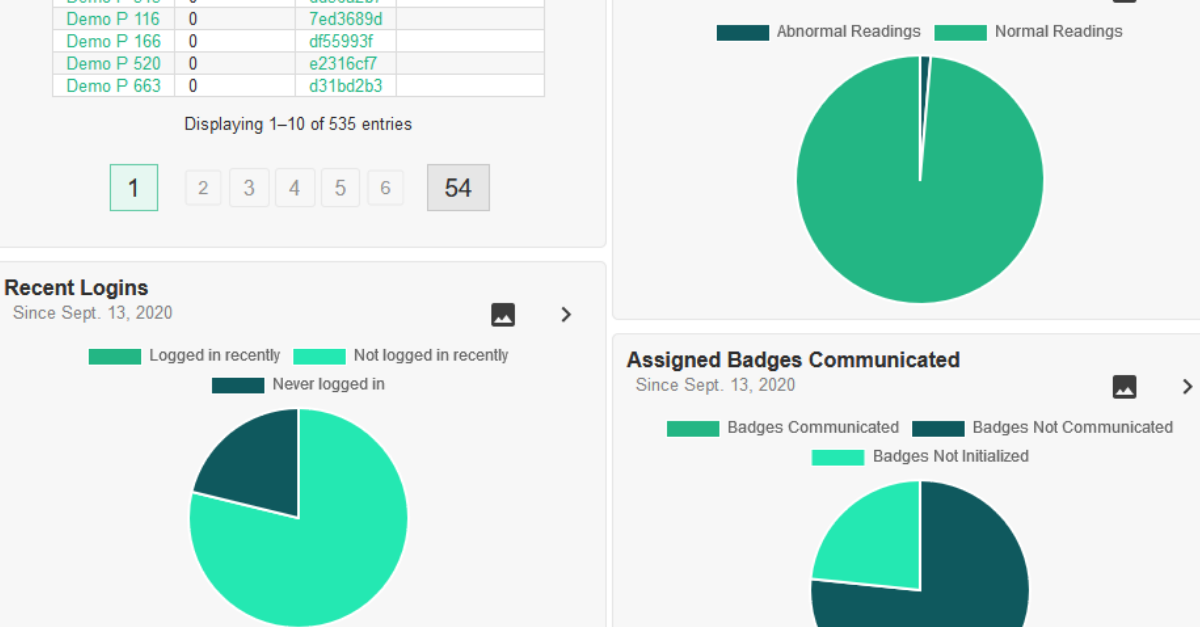
Katelyn 01:48: Yeah, absolutely. So, it is designed to help aid in the management of multiple accounts. So, whether those accounts are all through one vendor, being Mirion or Landauer, or if they’re from both vendors, this is very beneficial for managing those. You can change the dashboard, that’s what we’re currently looking at here for the module, and this dashboard is a quick at a glance view of your dosimetry account. And you can change what account you’re looking at from this first dropdown menu here that I’m hovering over currently, and you can also change it to look at specific locations or subaccounts, and that’s from the second dropdown menu here.
Additionally, we also have something called a Common Wearer Profile, and what that does is it’s going to combine dosimetry information from more than one account. So if you have a wearer that has a badge from both vendors, or maybe they have two badges that are under different locations or subaccounts, you can combine that information into one profile to make viewing that dosimetry history a lot easier for that wearer.
KB 02:50: So, if I wanted to add or remove any of those multiple badges on my account, can I do so from within Odyssey?
Katelyn 02:57: Yeah, great question. So, the actual addition or editing of any of the badges for wearers for your program will still take place in your vendor portal, whether that’s Mirion, Landauer, or another party. So this particular module is designed to give you some additional features that aren’t available in those vendor portals. Some of those features include ALARA reporting, easy form 5 access, different alerts and reminders, shipping, different management for some of those high-level activities that you’re going to need to do for your program.
KB 03:31: I see. What about this dashboard? Is it possible to change any of the information that’s displayed here?
Katelyn 03:38: Yes. I definitely recommend that when you start utilizing this module in the software that’s something you do right away because it makes it very beneficial for you, and you can do that by selecting this gear icon here, it’s going to take us to show us all of the settings. So each of these boxes we refer to as a widget, and each widget has its own settings for what you want to view on your dashboard. A good example here is the Recently Viewed widget in the top right-hand corner. I have what I want to see available for selection with these checkboxes, I have some drop-down menus for the number of things that I want to see here for the Read activity widget I can choose the time period… so depending on what it is they each have their own settings for these particular widgets, and that way you can really make it for what you need to see for your program.
In addition to that, you can also click and drag things to more prominently display them. So, if I want to have this graph of Read Activity–these are doses that are coming in each day–I can put this at the very top so I can see that a more prominent position. You can also hide things if they aren’t useful to your program. So, say you don’t want this recently viewed widget, I can select the eye icon and hide that and if I were to save these settings it would remove that from my dashboard. So, it’s very customizable.
KB 04:59: You mentioned read activity. Is there a place that I can see who hasn’t read their badge?
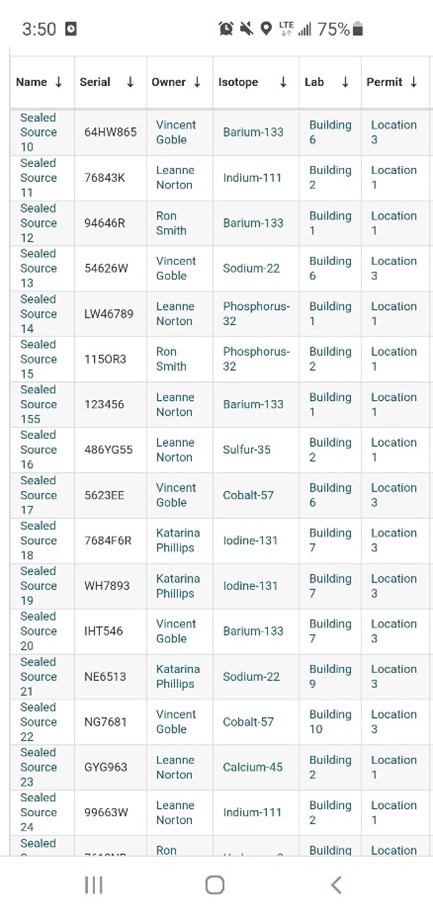
Katelyn 05:06: Yeah, so we have a query data section which I can actually go to and show you here. And this section allows you to do some really in-depth searches on your dosimetry data. You can choose to select what you want to search for, so with your example, I would go and search for different personnel, and ones that don’t have a badge reading. And then I come down to this section where it says Include or Exclude and I can choose things that I want to either include in my search or exclude from my search. And for us today, I’ll go ahead and add in an inclusion statement to include people for the current account that we’re looking at, just as an example, and then I can exclude people who have readings and we will only be left with those who do not, so I’ll go ahead and exclude people who have a reading for this year by putting in the date of January 1st.
So we can hit this play button here and it’s going to then search through all of your dosimetry records and give you the corresponding data for your filters. Once it does so, you have a table result at the bottom. And so, the format of this data is a little odd due to the fact that we’re looking at primarily, or not primarily, exclusively demo data. So you can see the employee IDs are very long. But this is what the format of that table would look like for you, just have your own dosimetry data displayed in it.
And these are linked to other areas of the software. So for these wearers, I can actually select them to go to their profiles, and in addition, we have a list of contact information here that if you were to select this mail icon for it would actually put all of these people into a mailing list for you so you can easily communicate with them. So if we do want to reach out to this group and say hey, you need to please read your badge for 2021, you can do so by this easy feature there.
KB 07:02: Well that seems pretty easy to do. Is there any way for me to receive notification of individuals with high doses?
Katelyn 07:10: Absolutely. So that is actually one of my favorite features that we have added into the Personnel Dosimetry module and it exists in this reporting section. So I’ll go ahead and select that and we’ll take a look at that.
The reporting section has a tab called ALARA. The module has the ability to add in different custom ALARA thresholds. For this particular demo dosimetry account, we have two thresholds added in. I’ve added in an ALARA 1 and an ALARA 2. These are both quarterly thresholds but you can also have them trigger on a single dose, they can be monthly, quarterly, or annually. So, you have a variety of options there. They can also be scoped to particular badge regions that a badge is assigned to. Since these are quarterly thresholds, this next filter of the period gives me the option to choose a quarterly time period but that will change depending on your threshold. And if I do put in last quarter as an example and select run report, what that’s going to do is give me a table of results of individuals that have surpassed that threshold for the chosen time period. So we have these three demo people who have surpassed the ALARA 1 Threshold, and then one person additionally also surpassed the ALARA 2, so this table is really nice because if they did surpass other thresholds it will let you know that. So if you only want to follow up on the higher of the two you absolutely can do that.
It will tell you the time period that we’re covering currently, and then the cumulative dose for that time period, and then the stage that you’re at in the process. So this will allow you to email each of these individual wearers either notification that they went over this dose threshold or a questionnaire – that form that they actually get sent is completely customizable – and the wearer will receive that via email. Once they do, they will open and view that, if they have any questions they can fill that out, it requires a signature and dates it for them automatically, and then that gets sent back to Odyssey. Once it does get sent back, this pie chart progresses and shows you where this process is. So it will change to being yellow for “waiting for RSO response.” So if you’re an RSO, a radiation safety representative, you can come in here, review that questionnaire, and the responses, and sign off on that to complete the process.
And to get back to your initial question about alerts for these items, throughout this entire process you’re going to be receiving in-software alerts which can optionally be email alerts as well. So when a wearer initially goes over the threshold, any of these thresholds you have set up, you’re going to get an alert that looks like a post-it note like one of these. And then when they fill it out they also will trigger an alert and it’ll let you know they have it filled out so that way you can come in and review that as soon as possible. And so you’re always going to be notified of each stage of the process there as this progresses.
KB 10:07: Well that all sounds great! Thanks, Katelyn, for helping us address some frequently asked questions about Odyssey’s Personnel Dosimetry module. Join both of us next week for part 2 where we’re going to be talking about the inventory tracking module and its ability to assist with tracking radioactive materials in your radiation safety program.
Katelyn 10:26: Thanks, KB.
Schedule an in-depth demo with our Odyssey team to discuss how the software can assist you with your radiation safety management needs or visit our website to learn more about Odyssey’s radiation safety modules.